Hormones and Headaches in Women: Expert Tips
Discover how hormones can trigger headaches in women and learn expert-backed tips for achieving lasting relief. Explore strategies for hormonal balance and enhancing your daily wellbeing.
Editor
5/15/20254 min read
Do you find yourself bracing for a headache at certain times of the month? Or perhaps you've noticed a shift in headache patterns as you've entered different life stages, like perimenopause or pregnancy? If so, you're not alone. For many women, there's a profound and often frustrating connection between their hormones and the frequency and intensity of headaches, particularly migraines. Understanding this link is the first step towards finding effective relief and improving your overall quality of life.
The Estrogen Enigma: Why Hormones Matter for Headaches
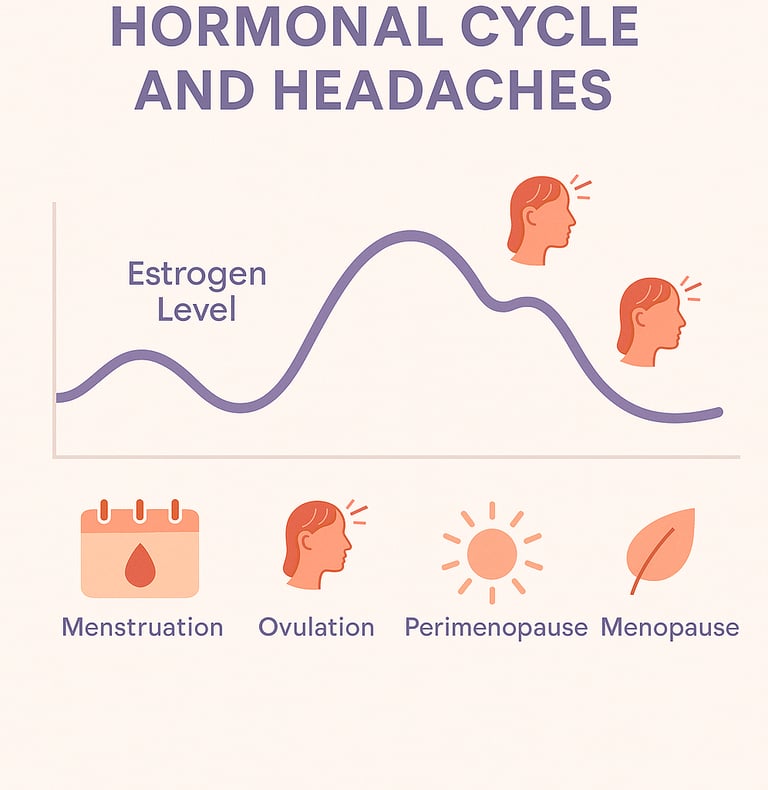
The primary hormonal player implicated in these headaches is estrogen. While the exact mechanisms are complex, fluctuations in estrogen levels, especially sudden drops, are believed to influence brain chemicals and blood vessels in ways that can trigger head pain.
The Menstrual Cycle: Many women experience "menstrual migraines" – headaches that typically occur in the days leading up to or during their period. This timing coincides with a natural sharp decline in estrogen levels.
Perimenopause: This transitional phase leading up to menopause is characterized by erratic and unpredictable hormonal fluctuations. These swings can trigger new onset headaches or worsen existing migraine patterns for some women.
Menopause: After menopause, estrogen levels are consistently lower. For some, this stability brings headache relief. However, others may continue to experience headaches, or even develop them if they start Hormone Replacement Therapy (HRT), as the type and dosage can influence headache patterns.
Pregnancy: Hormonal changes during pregnancy are significant. Many women with a history of migraine find their headaches improve, especially during the second and third trimesters when estrogen levels are high and stable. However, some may experience more headaches in the first trimester.
Oral Contraceptives and HRT: Depending on the type, dosage, and individual sensitivity, hormonal contraceptives and hormone replacement therapy can either improve, worsen, or have no effect on headaches. Pills that cause a sharp drop in estrogen during the placebo week can be problematic for some.
Taking Control: Lifestyle Strategies for Hormonal Headache Management
While you can't always control your hormonal fluctuations, you can adopt lifestyle strategies that may help reduce the frequency and severity of hormonally-triggered headaches:
Become a Headache Detective – Track Your Symptoms:
Keep a detailed headache diary. Note when headaches occur, their intensity, duration, and any accompanying symptoms. Crucially, correlate this with your menstrual cycle, dietary intake, sleep patterns, stress levels, and any medications. This data is invaluable for identifying personal triggers and patterns.
Nourish Your Body Wisely:
Eat Regularly: Skipping meals can cause blood sugar drops, a common headache trigger. Aim for balanced meals and snacks throughout the day.
Stay Hydrated: Dehydration is a major, yet often overlooked, headache culprit. Sip water consistently.
Identify Food Triggers: Common suspects include aged cheeses, processed meats (nitrates), chocolate, caffeine (or withdrawal), artificial sweeteners (like aspartame), and alcohol (especially red wine). Your diary will help pinpoint yours.
Consider Magnesium: This mineral plays a role in nerve function and blood vessel regulation. Some studies suggest magnesium supplementation can be beneficial for migraine prevention. Good food sources include leafy green vegetables, nuts, seeds, and whole grains.
Prioritize Restorative Sleep:
Maintain a Consistent Sleep Schedule: Go to bed and wake up around the same time each day, even on weekends, to regulate your body's natural rhythms.
Optimize Your Sleep Environment: Ensure your bedroom is dark, quiet, and cool. Limit exposure to blue light from screens before bedtime.
Master Stress Management:
Stress is a powerful headache trigger. Explore techniques like:
Mindfulness and Meditation: Even 10-15 minutes a day can make a difference.
Yoga or Tai Chi: Gentle, mindful movement can reduce tension.
Deep Breathing Exercises: A quick and effective way to calm your nervous system.
Regular Physical Activity: Aim for moderate exercise most days of the week, but be cautious as sudden, intense exertion can trigger headaches in some individuals.
Setting Boundaries: Learning to say "no" and protecting your time can significantly reduce stress.
Be Mindful of Caffeine:
While caffeine can help alleviate some headaches in the short term (it's an ingredient in many headache medications), regular high intake can lead to dependency and withdrawal headaches. If you consume caffeine, do so in moderation and consistently.
When to Seek Professional Guidance
While lifestyle modifications can be incredibly helpful, it's crucial to consult with your doctor or a healthcare professional, especially if:
Your headaches are new or have changed in pattern.
They are severe or debilitating.
They are accompanied by other concerning symptoms (e.g., fever, stiff neck, vision changes, numbness).
Over-the-counter medications aren't providing relief.
Your doctor can help confirm if your headaches are indeed hormonally related, rule out other potential causes, and discuss a range of treatment options. These might include specific acute medications to take at the onset of a headache, preventative medications, or adjustments to hormonal therapies if you are using them.
Understanding the interplay between your headaches and hormones is empowering. By tracking your symptoms, making informed lifestyle choices, and working with your healthcare provider, you can take significant steps towards managing your headaches and reclaiming your wellbeing.
References:
Calhoun, A. H. (2018). Understanding and treating menstrual migraine. Current Treatment Options in Neurology, 20(4), 11. DOI: 10.1007/s11940-018-0495-9
MacGregor, E. A. (2020). Menstrual and perimenopausal migraine. Practical Neurology, 20(1), 42-50. DOI: 10.1136/practneurol-2018-002159
Mauskop, A., & Varughese, J. (2012). Why all migraine patients should be treated with magnesium. Journal of Neural Transmission, 119(5), 575–579. DOI: 10.1007/s00702-012-0790-2
(Disclaimer: This blog post is for informational purposes only and does not constitute medical advice. The information provided is not intended to diagnose, treat, cure, or prevent any disease. Always seek the advice of your doctor with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this blog.)
Disclaimer
Content on HeadacheMama.com is for informational purposes only and is not a substitute for professional medical advice. Always consult your doctor.
contact@headachemama.com
© 2025. All rights reserved.